RPM (Remote Patient Monitoring) CPT codes are a way for healthcare providers to get reimbursed for monitoring patients' health remotely using digital devices. Think of it like having a virtual nurse keeping an eye on you between doctor visits. These codes cover the time spent setting up the monitoring devices, reviewing the data they collect, and communicating with patients about their health. It's like having an extra layer of support that helps doctors keep track of your health without you needing to be in the clinic all the time. This digital health solution not only enhances patient care but also presents an opportunity for healthcare providers to improve revenue generation. By efficiently utilizing remote patient monitoring, providers can optimize their time and resources which lead to increased patient volume, as monitoring remotely allows for more patients to be managed simultaneously. Ultimately, integrating RPM into clinical routines not only improves patient outcomes but also contributes to the financial sustainability of healthcare practices. Utilizing CPT codes 99457 and 99458 enables healthcare providers to further enhance revenue by accurately documenting and billing for the time spent on remote patient monitoring activities beyond the initial setup. These codes allow for transparent reimbursement for the additional time and effort invested in interpreting monitoring data and communicating with patients, thereby optimizing revenue streams within clinical routines.
This article discusses the formulation of automating patient prioritization for the clinical team in RPM as a Multi-arm Bandit problem involves viewing each patient as an "arm" representing a potential monitoring strategy. The proposed algorithm prioritizes patients in such a way that it tries to balance the motive of optimal patient care by ensuring enough time allocation and generating revenue out of potential patients aligning CPT billing norms. Therefore, this automation enhances time efficiency for clinical teams by allowing them to focus on providing high-quality patient care instead of spending time on patient prioritization, facilitating iterative improvements in revenue generation simultaneously. Before delving into the issue, the article first provides a brief overview of the relevant background topics.
Multi-Armed Bandit Problem
It is a classic problem in decision theory and reinforcement learning which is formulated based on a reward slot machine with multiple arms. A multi-armed bandit is a complicated slot machine wherein instead of 1, there are several levers which a gambler can pull, with each lever giving a different return. The goal of the problem is to repeatedly select one of the several actions in order to maximize the cumulative reward. To make the best out of this rewarding machine, we have to perform the series of actions with a sweet balance of exploration and exploitation. By design, this problem is the most straightforward example of exploration-exploitation dilemma we can think of and that’s the reason why it has been studied for so long and is still of first interest within the scientific community.
Exploration-Exploitation Tradeoff Dilemma
It is a metaheuristic process where the algorithm undergoes both exploring and exploiting phases to leverage the best out of the search space, which consists of all possible solutions and their quality. If the algorithm explores too much and considering its randomness, one misses the chance to find better solutions. On the other hand, if the algorithm gets caught up in the exploitation phase, there is a high chance of obtaining a sub optimal reward by missing out on information in the search space. Therefore, the algorithm needs to balance the trade-off to achieve a good compromise between quality and diversity of solutions. To facilitate this strategy, we are resorting to e-greedy algorithm i.e., Epsilon-Greedy algorithm.E-Greedy algorithm is the most naive yet incorporates exploration in a decision making process. The idea is simply to take either the action that seems to be optimal i.e., exploitation with the weightage e or a completely random action with the weightage (1-e) for exploration. This algorithm introduces parameter e to balance the exploitation and the exploration, a low value of e indicating a high degree of exploration. Thus, when the parameter e is equal to 0, the algorithm indulges in random acts of exploration whereas for value 1, the algorithm gets into greedy exploitation.
How CPT 99457 and 99458 work
RPM codes 99457 and 99458 are used for care management and coordination. Billing for code 99457 requires 20 minutes of patient-interactive virtual care during the calendar month by a qualified healthcare provider or care manager. The 20-minutes of intra-service work associated with CPT codes 99457 and 99458 includes a practitioner’s time engaged in “interactive communication” as well as time engaged in non-face-to-face care management services during the month.Furthermore CPT 99458 is also a part of the interactive virtual care during the calendar month. However, this code is for additional time spent with the patient. After meeting the requirements for code 99457, healthcare organizations can bill in additional 20-minute increments using code 99458. For example, if a patient gets 40 minutes of virtual care covered by RPM, this code will be used to bill for the incremental 20 minutes.
Mathematical Formulation
To delve into the mathematical underpinnings of our proposed time optimization strategy to prioritize patients for Remote Patient Monitoring, let's frame the problem in the context of a Multi-Armed Bandit (MAB) scenario.Based on the formulated scenario, we can consider each patient as an "arm" of the bandit, representing a potential candidate who achieves a 20 minute block to satisfy CPT billing criteria. Our goal is to systematically prioritize patients on a daily basis and allocate time accordingly to enhance patient care over the course of a month within our problem context.In the context of our proposed strategy for Remote Patient Monitoring (RPM), balancing exploration and exploitation is paramount to optimize monitoring time and revenue generation. During the exploration phase, we focus on patients for whom we have achieved fewer minutes of care by allocating clinical care time and assessing patient needs. This phase allows us to explore the diverse range of patient profiles and identify potentially lucrative monitoring opportunities. Conversely, in the exploitation phase, we prioritize patients who have already received some level of care, aiming to satisfy the 20-minute block requirement for billing CPT codes 99457 and 99458. By strategically transitioning between exploration and exploitation, we can iteratively refine our time allocation while ensuring high-quality patient care and compliance with billing regulations alongside revenue generation.To begin with, we introduce a novel variable "day factor" to influence the balance between exploration and exploitation phases.

By incorporating this dynamic parameter, we aim to adapt our time allocation strategy throughout the month by allocating clinical monitoring time for patients whom we achieved less duration during the exploration phase and satisfy the criteria by attending the patients who are close to the 20 minute block. From the following plot, it is observed that how the algorithm gets influenced by the weightage of exploration and exploitation over a period of month. We can summarize that our proposed prioritizing approach highly undergoes the exploration phase during the first half of the month and exploitation phase during the rest of the month.

The end goal of our problem is to monitor as many patients as possible for three blocks of 20 minutes i.e., 60 minutes in a month. Based on our problem’s end goal, we can formulate the expected time to attend each patient for at least 2 minutes a day over a month. This formulation ensures that each patient is expected to be monitored at least 2 minutes everyday throughout the month, aligning with the CPT billing norms. Also, we introduced the minimum function to ensure that the sum of expected attended minutes across days does not surpass 60, especially in months with 31 days. This mathematical constraint helps maintain the integrity of our scheduling system by capping the total attended minutes within a given time frame. Hence, we formulate our expected attended minutes for a day as follows:

To attain the objective of our problem, we have to prioritize the patients based on the time they were monitored and the phase our algorithm undergoes i.e., exploration and exploitation, during the day of the month. We make use of the epsilon-greedy optimization algorithm to generate priority values for each patient who is being monitored. To compute priority value, firstly we find the difference between the total minute particular patient Pminutes achieved was attended by clinical team and find the difference expected minute attended Eminutes achieved which is further normalized between 0 and 1 to calculate minutes the patient lags or leads on the particular day.

Additionally, we aim to assess how close the patient's current progress is to achieving the 20-minute milestone:

After computing the farness and proximity between minutes achieved for a patient and 20-minute block, we are all set to calculate the priority value for each patient. As our proposed approach tries to balance the exploration and exploitation phase day-to-day , the e-greedy algorithm generates priority values Qvalue for the patient by taking into account both the farness and proximity with the weightage on a particular day of the month.

Overall, our formulation provides a robust mathematical foundation for optimizing revenue in RPM, taking into account factors such as patient monitoring duration, algorithmic phase, and billing criteria to ensure efficient resource allocation and high-quality patient care.
Mathematical Formulation
In our effort to demonstrate the practical application of our problem formulation for in patient prioritization, we have developed a tabular and chart demonstration through which readers can get insightful evidence of how this proposed approach would ease the clinical team in prioritizing the pool of patients effortlessly.To begin with, a synthetic dataset was created, featuring two distinct columns: "Patient ID," consisting of randomized alphanumeric strings ranging from five to ten digits, and "minutes_attended," where values were randomly allocated within the interval of 3 to 32 for each corresponding patient ID. The demonstrated dataset which we created is presented as follows with a sample of ten patients.

To validate our methodology, we put into practice the framework we proposed by developing it in the Python programming language. Through this implementation, we computed the priority value corresponding to each patient across various days of the month. The outcomes of this computational analysis are organized and displayed in tabulated form, facilitating a clear presentation of the generated priority values for each patient on different days throughout the month.
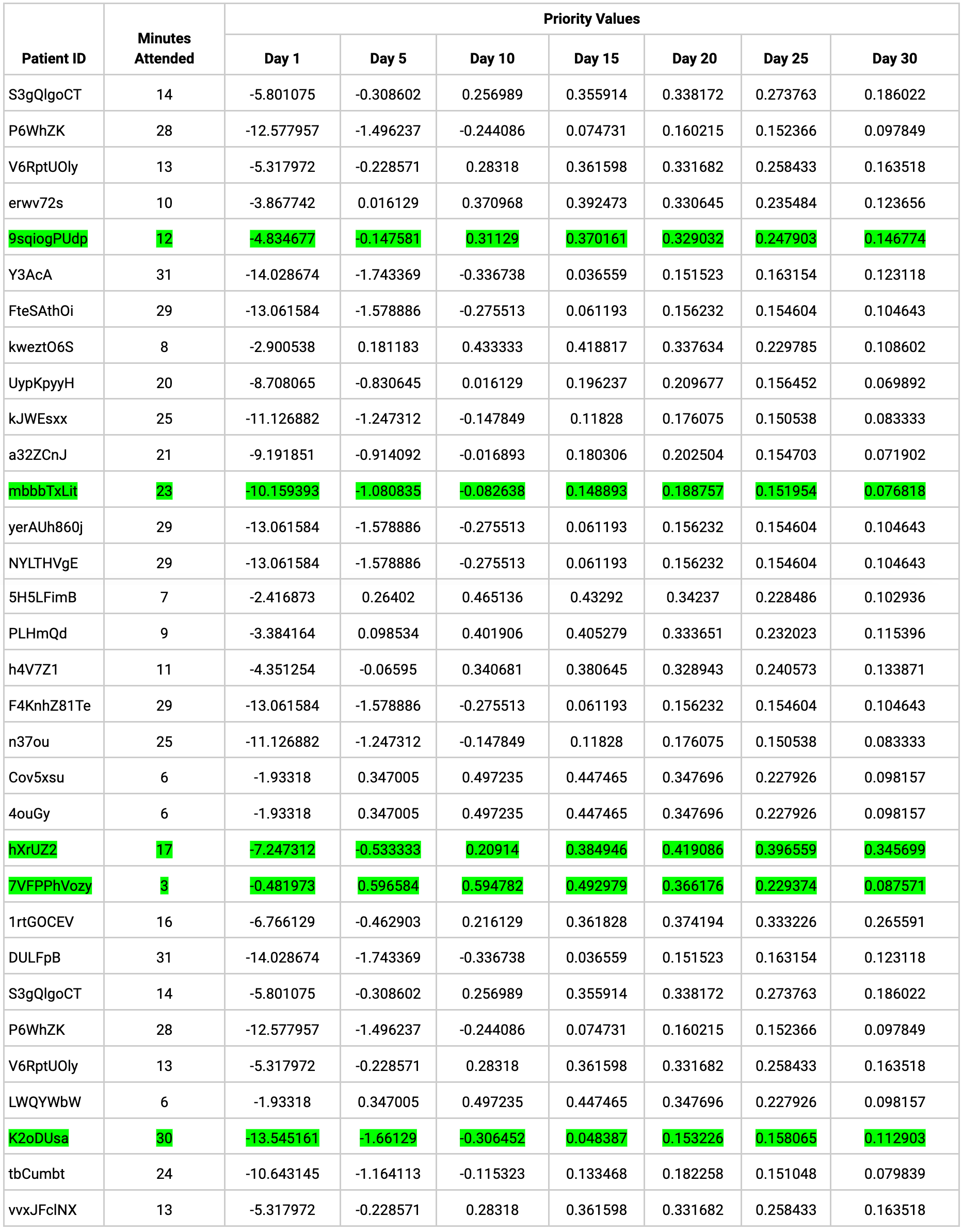
The tabular data may appear convoluted and challenging to interpret, right? For better clarity and more intuitive understanding, a subset of five patients was selected based on their attendance minutes. This deliberate selection aimed to encompass various scenarios, including corner cases, to cover different situations, even the tricky ones, to help explain how our algorithm maintains the exploration and exploitation balance. These are the patients whom we have chosen to visualize their priority ranking over a month.

ID 7VFPPhVozy: In this instance, the clinical team spent only 3 minutes attending to the patient. Our prioritization algorithm aims to target patients who receive minimal attention, particularly in the early days of the month. The line chart illustrates a high priority ranking during the first half of the month, followed by a gradual decline in priority. This declining trend reflects a diminishing level of significance assigned to the patient due to their limited time attended.ID 9sqiogPUdp: The patient's priority ranking exhibits fluctuations, with periods of both elevation and decline, suggesting varying levels of importance or attention directed towards them. Despite this variability, the algorithm aims to ensure the patient reaches the 20-minute billing block by prioritizing them towards the end of the month, as their attended time only amounts to 12 minutes.
ID hXrUZ2: The patient received 17 minutes of attention, nearing the 20-minute billing block threshold. The line chart illustrates consistent low priority for this patient during exploration and a shift to high priority during exploitation. Throughout the month, the algorithm effectively balances exploration and exploitation by prioritizing revenue-generating patients while also allocating time to those who have received less attention.
ID mbbbTxLit: The patient received 23 minutes of attention, effectively meeting the 20-minute billing block required by CPT norms. Initially, our algorithm prioritized such cases at the start of the month for extra care. However, as the month progressed, it adjusted priorities, giving lower precedence to this patient to focus on others nearing the 20-minute billing threshold, as detailed in the subsequent discussion on patient ranking, particularly for the patient with ID K20Dusa.
IDK20Dusa: In our synthetic dataset, this patient received only 30 minutes of attention, leading the algorithm to assign them the lowest priority among 25 patients for nearly 20 consecutive days within the month. However, recognizing the need to optimize patient care, the algorithm adjusted its priorities, ultimately granting the patient a higher priority status to ensure they received additional attention. This decision aimed to maximize the utilization of available time by allocating another 20-minute block for additional revenue generation from this patient.
Conclusion
The proposed approach for automated patient prioritization, with the balanced motive of optimal patient care and revenue generation, in RPM using a Multi-Arm Bandit framework provides a structured method for clinical teams to allocate their resources efficiently, improving time management while maintaining high-quality patient care. By viewing each patient as a potential strategy for monitoring, healthcare providers can dynamically adjust their attention and time allocation to maximize time efficiency, effectively balancing setup, monitoring, and communication efforts. The mathematical formulation and analysis showcased in the blog highlight the efficacy of this approach in enhancing time efficiency while ensuring optimal patient outcomes. This strategic integration of patient prioritization within RPM and the Multi-Arm Bandit framework not only improves healthcare practices but also enhances the sustainability and efficiency of clinical routines in the digital health landscape.


